|
---------------------------- 2020 Platform Presentation Winner --------------------------
[1092] Loss of MHC Class I Expression in PD-L1-positive HPV-Associated Cervical and Vulvar Neoplasia: A Mechanism of Resistance to Checkpoint Inhibition?
Megan Dibbern1, Timothy Bullock2, Linda Duska2, Mark Stoler3, Anne Mills2
Background: Decreased expression of major histocompatibility complex class I (MHC I) on tumor cells precludes antigen presentation and therefore prevents immune recognition. Alterations in MHC I expression are thought to compound immune escape and contribute to immunotherapeutic resistance in PD-L1-positive gastric and non-small cell lung carcinomas, but this has not been previously studied in cervical and vulvar cancers. Given the recent FDA approval of anti-PD-1 checkpoint inhibition in PD-L1-positive cervical squamous carcinomas, identifying tumors with loss of MHC I is of clinical interest.
Design: Immunohistochemistry for PD-L1 and MHC I combined A-, B-, and C- heavy chains was assessed in 58 HPV-associated cervical and vulvar lesions, including squamous intraepithelial lesions (SIL) and invasive squamous cell carcinoma (SCC) (15 CIN3, 13 cervical SCC, 12 VIN3, and 18 vulvar SCC cases). PD-L1 expression was classified as present or absent using the combined positive score (CPS) with a threshold of ≥1 required for positivity. MHC I staining was classified as present, clonally lost, or absent.
Results: Although 83.9% of SCC and 22.2% of SIL were PD-L1-positive, 33.5% (11/31) of SCC and 18.5% (5/27) of SIL also showed clonal or complete loss of MHC Class I. Loss of MHC I expression was more common in PD-L1-positive 10/26, 38.5%) vs. PD-L1-negative SCC (1/5, 20%). Among PD-L1-positive SCC, loss of MHC I expression is more common in cervical SCC (5/11, 45.5%) than vulvar SCC (5/15, 33.3%). However, neither of these differences was statistically significant.
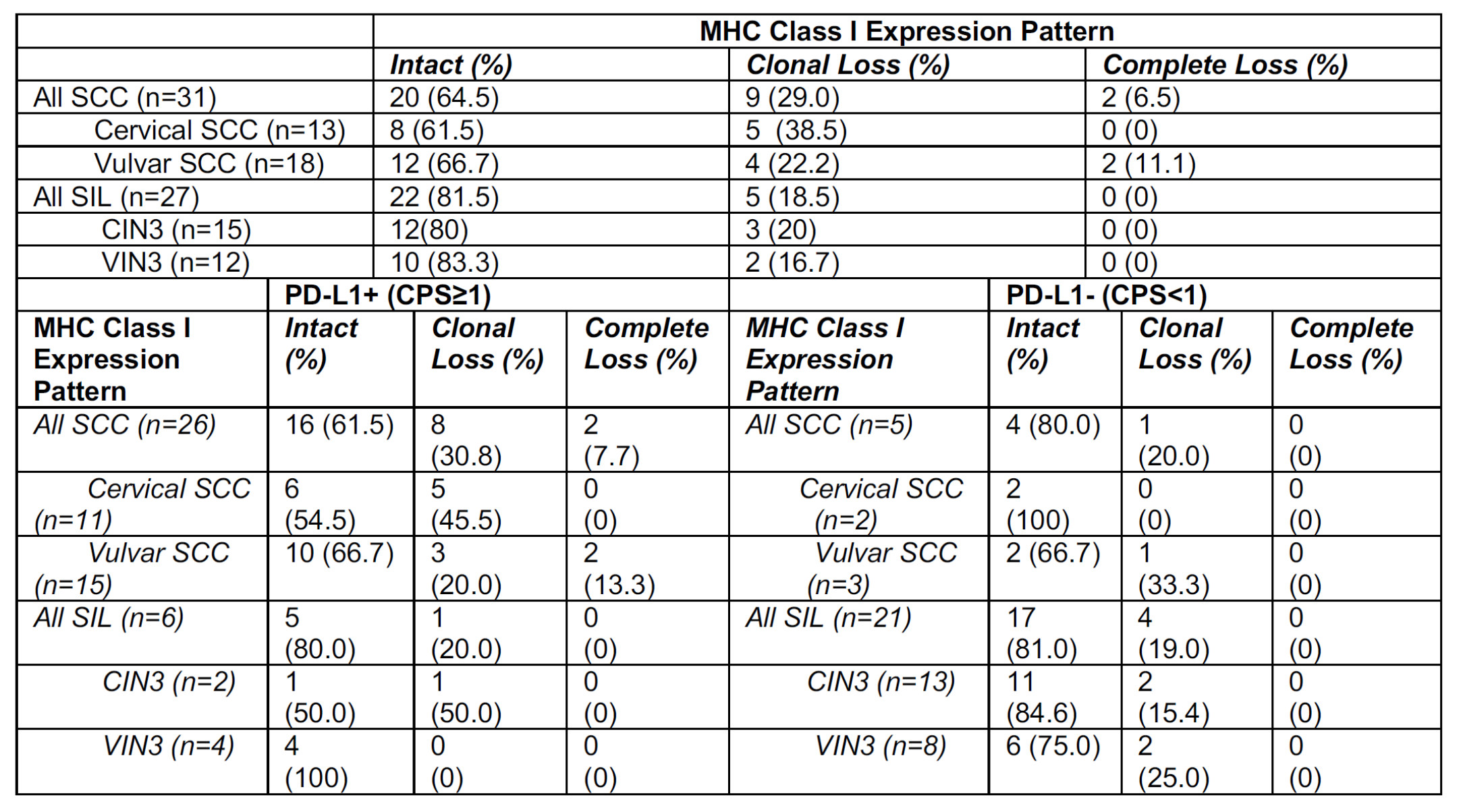
Conclusions: Over one-third of HPV-associated cervical and vulvar SCC show clonal or complete loss of MHC I expression. This suggests that response to therapies targeting the PD-1/PD-L1 axis may be inhibited in a subset of cervical and vulvar neoplasms due to an impaired ability to engage with the immune system related to loss of MHC Class I expression.
|