|
---------------------------- 2021 Platform Presentation Winner (shared) --------------------------
[551] Clinicopathologic and Molecular Prognostic Factors in FIGO Stage I Uterine Leiomyosarcoma: Interim Analysis of a Large Population-Based Cohort
David Chapel, Annacarolina Da Silva, Bradley Quade, Marisa Nucci
Background: Previous work has implicated patient age, tumor size, circumscription, histotype (spindled, epithelioid, myxoid), cytologic atypia, mitotic count, lymphovascular invasion, hormone receptor status, and recurrent copy number alterations as prognostic factors in FIGO stage I uterine leiomyosarcoma (uLMS). However, these factors have not been validated by multivariate modeling of a large cohort.
Design: We analyzed 15 clinical, morphologic, and immunophenotypic parameters in 149 stage I uLMS diagnosed between 2005-2020. Thirteen tumors were evaluated by a 447-gene targeted next-generation sequencing panel. Each clinicopathologic parameter and recurrent molecular alteration was evaluated by the log-rank test for overall (OS) and disease-free survival (DFS). Parameters significant on univariate analysis were included in a multivariate Cox proportional hazards regression model.
Results: Median OS was 85 months, with 61 (41%) patients dying over a follow-up ranging from 6-234 (median, 46) months. Median DFS was 30 months, with subsequent recurrence in 77 (57%) of 135 patients achieving clinical disease-free status. On univariate analysis, shorter OS and shorter DFS were significantly associated with coagulative necrosis, higher mitotic count, and positive margins (Figure 1). Homozygous RB1 deletion was associated with shorter OS (P=0.01), whereas larger tumor size and ATRX mutation were associated with shorter DFS (P=0.0004 & 0.04, respectively). Age, stage IA vs IB, histotype, cytologic atypia, lymphovascular invasion, infiltrative growth, and hormone receptor status were not associated with OS or DFS. On multivariate analysis, positive margins, higher mitotic count, and necrosis were independently associated with shorter OS and DFS, and larger tumor size was independently associated with shorter DFS. (Molecular parameters were excluded from multivariate modeling due to low numbers.
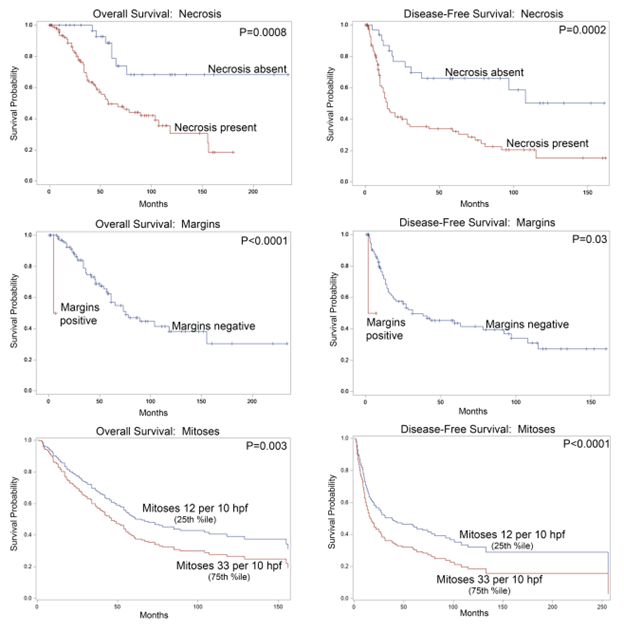
Conclusions: Multiple commonly evaluated morphologic parameters are independently associated with OS and DFS in stage I uLMS, including margin status, mitotic count, and coagulative necrosis. Tumor size is also independently associated with DFS. These parameters are clinically significant and should be routinely evaluated and reported for stage I uLMS. Certain molecular alterations, including RB1 deletion and ATRX mutation, are associated with shorter survival, but require further accrual for validation in multivariate models.
|